Aging and Sleep
- Circadian rhythms change as people age, often leading to disrupted sleep patterns.
- Increased prevalence of mental and physical health conditions can increase risk of fragmented sleep.
- Sleep disturbances can decrease sleep quality and quantity and become chronic sleep issues if not addressed.
- Improving sleep hygiene and developing healthy habits can encourage better sleep.
Aging is tied to numerous health concerns. Poor sleep can contribute to many of these problems, reducing quality of life in people as they get older.
In order to address the unique needs of older adults, it is more important than ever to understand the effects of aging on sleep and overall health. We take a closer look at the relationship between aging and sleep, common sleep issues, and sleep tips for older adults.
Why Does Aging Affect Sleep?
It is common for older adults to experience changes in the quality and duration of their sleep. Many of these changes occur due to changes in the body’s internal clock. Located in a part of the brain called the hypothalamus, this internal clock is made of around 20,000 cells that form the suprachiasmatic nucleus (SCN).
The SCN controls 24-hour daily cycles, called circadian rhythms. These circadian rhythms influence when people get hungry, when the body releases certain hormones, and when a person feels sleepy or alert.
As people get older, their sleep changes due to effects of an aging SCN . Deterioration in the function of the SCN can disrupt circadian rhythms, directly influencing when people feel tired and alert.
The SCN receives information from the eyes, and light is one of the most powerful cues for maintaining circadian rhythms. Unfortunately, research shows that many older people have insufficient exposure to daylight, averaging around one hour each day. Daylight exposure may be even more restricted for people who live in nursing homes as well as those with Alzheimer’s disease.
Changes in production of hormones, such as melatonin and cortisol, may also play a role in disrupted sleep in older adults. As people age, the body secretes less melatonin, which is normally produced in response to darkness and helps promote sleep by coordinating circadian rhythms.
Health Conditions and Sleep
Mental and physical health conditions may also interfere with sleep. Conditions that commonly affect sleep in older people include depression, anxiety, heart disease, diabetes, and conditions that cause discomfort and pain, such as arthritis.
The relationship between physical health and sleep is complicated by the fact that many older adults are diagnosed with more than one health condition. Those with multiple health conditions are more likely to report getting less than six hours of sleep, having poor sleep quality, and experiencing symptoms of a sleep disorder.
Sleep issues may also be related to the side effects of medications. Almost 40% of adults over the age of 65 take five or more medications. Many over-the-counter and prescription drugs can contribute to sleep issues. The interactions of multiple medications may also cause unanticipated effects on sleep.
Lifestyle and Sleep
Poor sleep quality in older adults can be related to the lifestyle changes that often come with aging. For example, retirement may lead to a less structured sleep-wake schedule. Other significant life changes, such as loss of independence and social isolation, can increase stress and anxiety, which can also contribute to sleep issues.
How Does Aging Affect Sleep?
Aging affects people differently. While some older adults may have no significant disruptions in their sleep, others complain about getting less sleep and having worse sleep quality. Experts have found several common sleep disturbances in older adults.
- Shifting sleep schedule: As people age, the body’s circadian rhythms actually shift forward in time. This shift is called a phase advance. Many older adults experience this phase advance as getting tired earlier in the afternoon and waking up earlier in the morning.
- Waking up at night: Research has also shown that as people get older, they often experience changes in their sleep architecture. Sleep architecture refers to how people cycle through the different stages of sleep. Older adults spend more time in the earlier, lighter stages of sleep and less time in the later, deeper stages. These shifts may contribute to older people waking up more often during the night and having more fragmented, less restful sleep.
- Longer recovery from changes in sleep schedule: Alterations in how the body regulates circadian rhythms make it more difficult for older people to adjust to sudden changes in their sleep schedules, like during daylight saving time or when experiencing jet lag.
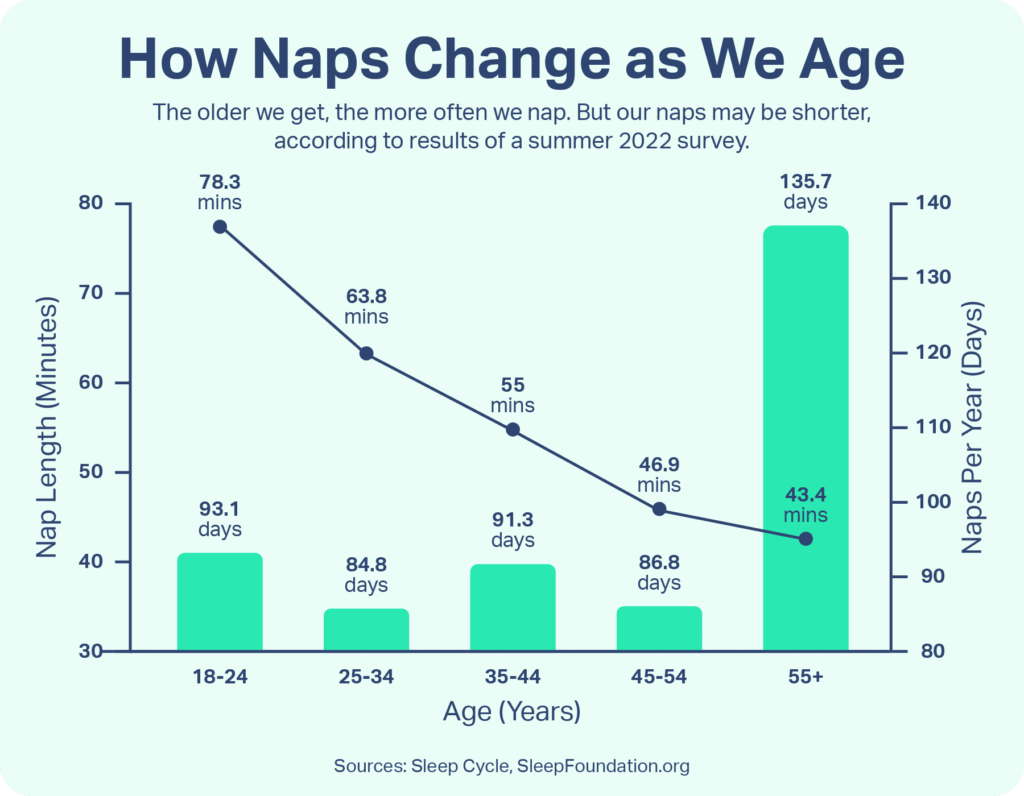
- Daytime napping: Research estimates that about 25% of older adults take naps, compared with around 8% of younger adults . While some experts suggest that a short daytime nap may be beneficial, many agree that extended napping and napping later in the day can make it harder to fall asleep at bedtime and create nighttime sleep disruptions.
Do Older People Need Less Sleep?
It is a common misconception that older adults require less sleep than younger individuals. Many older adults have a hard time getting the sleep they need, but that does not mean they need less sleep. In general, adults should aim to get at least seven hours of sleep each night.
Common Sleep Issues in Older Adults
Researchers estimate that between 40% and 70% of older adults have chronic sleep issues and up to half of cases may be undiagnosed . Chronic sleep problems can significantly interfere with older adult’s daily activities and reduce their quality of life. There are several sleep issues that are especially common in older adults.
- Pain: Discomfort and pain can lead to inadequate rest for some older adults. Pain and sleeplessness can become a vicious cycle, in which less sleep can lead to more pain. It is important to talk to a doctor if pain is interfering with sleep.
- Nighttime Urination: Nighttime urination, also called nocturia, increases with age due to physical changes in the urinary system and other factors. This issue may affect up to 80% of older adults , contributing to increased sleep disruptions.
- Insomnia: Having persistent difficulty in falling or staying asleep is one of the most common sleep issues in older adults. Insomnia may be caused by a variety of overlapping factors but can get better with treatment.
- Daytime Drowsiness: Many people believe that feeling tired during the day is a normal part of getting older, but this is not the case. Around 20% of older people experience excessive daytime sleepiness, which may be a sign of an underlying health condition. Excessive daytime sleepiness in older adults may be a symptom of health issues like sleep apnea, cognitive impairment, or cardiovascular issues.
- Sleep Apnea: Obstructive sleep apnea can cause pauses in breathing during sleep. These pauses are related to the upper airway collapsing or narrowing. Sleep apnea causes fragmented sleep and can affect oxygen levels in the body, leading to headaches, daytime sleepiness, and difficulty thinking clearly.
- Restless Legs Syndrome: Restless legs syndrome (RLS) affects 9% to 20% of older people , while periodic limb movement disorder (PLMD) affects 4% to 11%. RLS causes an urge to move the legs while resting or sleeping. PLMD causes involuntary movements in the lower limbs, most commonly in the feet.
- REM Sleep Behavior Disorder: REM sleep behavior disorder (RBD) primarily affects older people. While most people’s bodies do not move while they are dreaming, this disorder can cause people to physically act out their dreams, sometimes violently.
Sleep Tips for Older Adults
Research has shown that older people can take steps to improve their sleep. These steps often involve focusing on improving sleep hygiene and developing habits that encourage quality sleep.
- Exercise: Older people who exercise regularly fall asleep faster, sleep longer, and report better quality of sleep. Exercise is one of the best things older people can do for their health.
- Reduce bedroom distractions: Televisions, smartphones, and bright lights can make it more challenging to fall asleep. Keep the television in another room and try not to fall asleep with it turned on. Move electronics out of the bedroom and reserve the bedroom for only sleeping and sex.
- Avoid substances that discourage sleep: Substances like alcohol, tobacco, caffeine, and even large meals late in the day can make sleep more challenging. Consider quitting smoking, reducing caffeine intake, and eating dinner at least four hours before bedtime.
- Keep a regular sleep schedule: Aging can make it more difficult to recover from lost sleep. Avoid sudden changes in sleep schedules. This means going to bed and waking up at the same time every day and being careful about napping too long or too close to bedtime.
- Develop a bedtime routine: Find activities that help you relax before bed. Many older people enjoy taking a warm bath, reading, or finding some quiet time before getting into bed.
Safe Sleeping for Older Adults
As people age, it is helpful to make changes to the bedroom environment that reduce the risk of falls and accidents and makes it easier to call for help when needed. There are several steps that older adults can take for a safer night’s sleep.
- Keep a phone by the bed: It is important to be able to call for help from bed. Put a phone on the nightstand and keep a list of important phone numbers nearby. But be careful about keeping a smartphone nearby, particularly if it receives too many notifications during the night or if there is too much temptation to look at the bright screen.
- Make sure a light is within reach: Having a light easily accessible reduces the risk of stumbling, tripping, or falling in the dark when getting out of bed. Lights with motion sensors may be helpful in hallways or the bathroom.
- Reduce hazards in the bedroom: Never smoke in bed and be careful when placing objects in the bedroom that may become trip hazards, like rugs, cords, stools, and furniture. It is safest to have a clear path from the bed to the door.
References
8 Sources
-
National Institute of General Medical Sciences. (2022, March 11). Circadian rhythms., Retrieved February 22, 2023, from
https://www.nigms.nih.gov/education/fact-sheets/Pages/circadian-rhythms.aspx -
Li, J., Vitiello, M. V., & Gooneratne, N. S. (2018). Sleep in Normal Aging. Sleep Medicine Clinics, 13(1), 1–11.
https://pubmed.ncbi.nlm.nih.gov/29412976/ -
Stepnowsky, C. J., & Ancoli-Israel, S. (2008). Sleep and Its Disorders in Seniors. Sleep medicine clinics, 3(2), 281–293.
https://pubmed.ncbi.nlm.nih.gov/19122865/ -
Charlesworth, C. J., Smit, E., Lee, D. S., Alramadhan, F., & Odden, M. C. (2015). Polypharmacy Among Adults Aged 65 Years and Older in the United States: 1988-2010. The journals of gerontology. Series A, Biological sciences and medical sciences, 70(8), 989–995.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4573668/ -
Monk, T. H., Buysse, D. J., Carrier, J., Billy, B. D., & Rose, L. R. (2001). Effects of afternoon “siesta” naps on sleep, alertness, performance, and circadian rhythms in the elderly. Sleep, 24(6), 680–687.
https://pubmed.ncbi.nlm.nih.gov/11560181/ -
Miner, B., & Kryger, M. H. (2017). Sleep in the Aging Population. Sleep medicine clinics, 12(1), 31–38.
https://pubmed.ncbi.nlm.nih.gov/28159095/ -
Duffy, J. F., Scheuermaier, K., & Loughlin, K. R. (2016). Age-related sleep disruption and reduction in the circadian rhythm of urine output: Contribution to nocturia? Current Aging Science, 9(1), 34–43.
https://pubmed.ncbi.nlm.nih.gov/26632430/ -
Hornyak, M., & Trenkwalder, C. (2004). Restless legs syndrome and periodic limb movement disorder in the elderly. Journal of psychosomatic research, 56(5), 543–548.
https://pubmed.ncbi.nlm.nih.gov/15172211/










