When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
Sleep Paralysis: Symptoms, Causes, and Treatment
- Sleep paralysis is a brief loss of muscle control just after falling asleep or before waking up.
- Sleep paralysis frequently involves hallucinations or a feeling of suffocation.
- No one knows exactly what causes sleep paralysis, but it is linked to sleep disorders and certain mental health conditions.
Sleep paralysis is a temporary inability to move or speak that occurs directly after falling asleep or waking up. While the states of sleep and wakefulness are usually clearly defined and distinct, conditions like sleep paralysis can blur these boundaries. Individuals maintain consciousness during episodes, which frequently involve troubling hallucinations and a sensation of suffocation.
While much is still unknown about sleep paralysis, learning about types, symptoms, causes, impacts, and treatment can enable a better understanding of the condition and ways to prevent it.
Is Your Sleep a Problem?
Sleep Paralysis can be indicative of larger issues such as sleep apnea. Answer three questions to understand if you should be concerned.
What Is Sleep Paralysis?
Sleep paralysis is a condition marked by a brief loss of muscle control, known as atonia , that happens just after falling asleep or before waking up. In addition to atonia, people often experience hallucinations during episodes of sleep paralysis.
Sleep paralysis is considered a parasomnia, which are abnormal behaviors during sleep. Because it is linked to the rapid eye movement (REM) stage of the sleep cycle, sleep paralysis is considered to be a REM parasomnia. While standard REM sleep involves vivid dreaming along with atonia, both typically end upon waking up, so a person never becomes conscious of this inability to move.
As a result, researchers believe that sleep paralysis involves a mixed state of consciousness that blends both wakefulness and REM sleep. In effect, the atonia and mental imagery of REM sleep seems to persist even into a state of being aware and awake.
Types of Sleep Paralysis
Medical experts typically group sleep paralysis cases into two categories .
- Isolated sleep paralysis: These one-off sleep paralysis episodes are not connected to an underlying diagnosis of narcolepsy, a neurological disorder that prevents the brain from properly controlling wakefulness, which often leads to sleep paralysis.
- Recurrent sleep paralysis: This condition involves multiple sleep paralysis episodes over time. Recurrent sleep paralysis can be associated with narcolepsy.
In many cases, these two defining characteristics are combined to describe a condition called recurrent isolated sleep paralysis (RISP), which involves ongoing instances of sleep paralysis in someone who does not have narcolepsy.
What Does Sleep Paralysis Feel Like?
The defining symptom of sleep paralysis is atonia, or the inability to move the body or speak. People also report difficulty breathing, chest pressure, and distressing emotions like panic or helplessness during sleep paralysis episodes. It is common to feel excessively sleepy or fatigued the day after experiencing sleep paralysis.
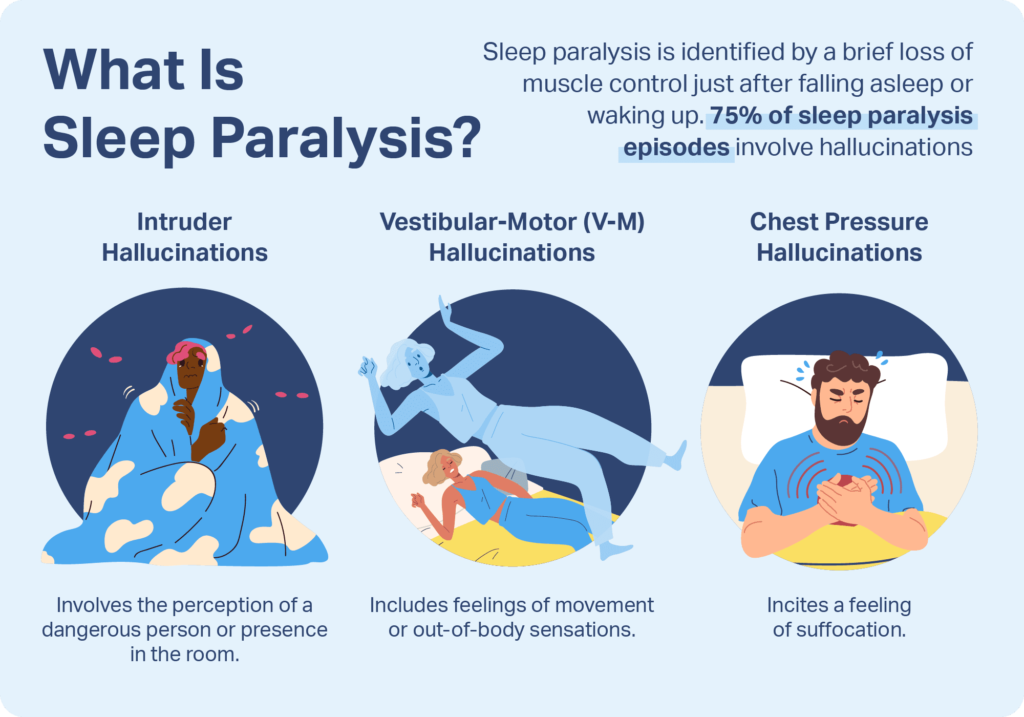
An estimated 75% of sleep paralysis episodes also involve hallucinations that are distinct from typical dreams. These can occur as hypnagogic hallucinations when falling asleep or as hypnopompic hallucinations when waking up.
Hallucinations during sleep paralysis fall into three categories.
- Intruder hallucinations: These hallucinations involve the perception of a dangerous person or presence in the room.
- Chest pressure hallucinations: Also called incubus hallucinations, these episodes may incite feelings of suffocation or the sensation that someone is sitting on your chest. These frequently occur in tandem with intruder hallucinations.
- Vestibular-motor (V-M) hallucinations: V-M hallucinations can include feelings of movement, such as flying, or out-of-body sensations.
How Common Is Sleep Paralysis?
Prevalence varies, but researchers believe that about 20% of people experience sleep paralysis at some point in their life. There is little data among this group about how often episodes recur. Sleep paralysis can occur at any age, but first symptoms often show up in childhood, adolescence, or young adulthood. After starting during teenage years, episodes may occur more frequently in a person’s 20s and 30s.
Episodes can last from a few seconds to 20 minutes, and the average length is around six minutes . In most cases, episodes end on their own but occasionally are interrupted by another person’s touch or voice, or by intense effort to move that overpowers atonia.

Does Sleep Paralysis Have Any Meaning?
The perception of sleep paralysis episodes has been found to vary significantly based on a person’s cultural context . Atonia is often distressing, and troubling hallucinations can make episodes even more disturbing. For this reason, around 90% of episodes are associated with fear, while only a minority have more pleasant or even blissful hallucinations.
Sleep paralysis has been interpreted differently across various spiritual and cultural beliefs. To some, sleep paralysis may be considered as a sign of something malevolent targeting you. To others, it may be considered a sign of spiritual awakening. Interpretations vary widely, but negative experiences during sleep paralysis have led to many stories and myths about sleep demons.
What Causes Sleep Paralysis?
The exact cause of sleep paralysis is unknown. Studies have analyzed data to determine what heightens one’s risk of sleep paralysis, and have found mixed results. Based on those findings, researchers believe that multiple factors are involved in the onset of sleep paralysis.
Sleep Disorders
Sleep disorders and other sleeping problems have shown some of the strongest correlations with isolated sleep paralysis. Higher rates of sleep paralysis — 38% in one study — are reported by people with obstructive sleep apnea (OSA), a sleep disorder marked by repeated lapses in breathing. Sleep paralysis also has been found to be more common in people with chronic insomnia, circadian rhythm dysregulation and nighttime leg cramps.
Narcolepsy
A pattern of multiple instances of sleep paralysis over a period of time may be connected to narcolepsy. Narcolepsy can alter the function of neurotransmitters in the brain, which may cause complications during REM sleep, including sleep paralysis. While roughly 20% of the general population experiences infrequent bouts of sleep paralysis, episodes are generally more frequent in those with narcolepsy. Consider speaking with your doctor if you experience signs of narcolepsy, including episodes of falling asleep without warning at inappropriate times, excessive daytime sleepiness, or muscle weakness.
Mental Health Disorders
Certain mental health conditions have shown a connection to sleep paralysis. Some of the strongest associations are in people with post-traumatic stress disorder (PTSD) and others who have been exposed to physical and emotional distress. Those with anxiety disorders, including panic disorder, also appear to be more likely to experience the condition. Stopping alcohol or antidepressants can lead to REM rebound, which may also cause sleep paralysis. Studies have found a higher risk in people with a family history of sleep paralysis, but no specific genetic basis has been identified.
Dream Patterns
Some studies have found that people who show traits of imaginativeness and disassociation from their immediate environment, such as daydreaming, are more likely to experience sleep paralysis. There may be a link as well between sleep paralysis and vivid nightmares or lucid dreaming. Further research is necessary to investigate these correlations and better understand the numerous potential causes of sleep paralysis.
Is Sleep Paralysis Dangerous?
For most people, sleep paralysis is not considered dangerous. Though it may cause emotional distress, it is classified as a benign condition and usually does not happen frequently enough to cause significant health effects.
However, an estimated 10% of people have more recurrent or bothersome episodes that make sleep paralysis especially troubling. As a result, they may develop negative thoughts about going to bed, reducing time allotted for sleep or provoking anxiety around bedtime that makes it harder to get restful sleep. This resulting sleep deprivation can lead to excessive daytime sleepiness and numerous other consequences for a person’s overall health.
What Are the Treatments for Sleep Paralysis?
Overall, there is limited scientific evidence about the most effective treatment for sleep paralysis. Many people are unaware that the condition is relatively common and thus feel ashamed after episodes. As a result, acknowledgment and normalization of their symptoms by a doctor can be beneficial.
Because of the connection between sleep paralysis and general sleeping problems, improving sleep hygiene is a common focus in preventing sleep paralysis. A first step in treating sleep paralysis is speaking with a doctor in order to identify and address underlying problems that may be contributing to the frequency or severity of episodes.
There are a number of sleep hygiene techniques that can contribute to better sleep quality and more consistent nightly rest.
- Establish a routine: Follow the same schedule for going to bed and waking up every day, including on weekends. A soothing pre-bed routine can help you get comfortable and relaxed.
- Optimize your sleep space: Outfit your bed with the best mattress and pillow for your needs. It is also useful to design your bedroom to have limited intrusion from light or noise.
- Curb substance use: Reduce alcohol and caffeine intake, especially in the evening.
- Remove distractions: Put away electronic devices, including smartphones, for at least an hour before bed.
Improving sleep hygiene is frequently incorporated into cognitive behavioral therapy for insomnia (CBT-I), a type of talk therapy that works to reframe negative thoughts and emotions that detract from sleep. CBT has an established track record in addressing mental health conditions. A specific form of CBT has been developed for sleep paralysis , but more research is needed to validate its effectiveness.
References
11 Sources
-
Brooks, P. L., & Peever, J. H. (2008). Unraveling the mechanisms of REM sleep atonia. Nature and Science of Sleep, 10, 355-367.
https://pubmed.ncbi.nlm.nih.gov/19226735/ -
Zhang, W., & Guo, B. (2018). Freud’s dream interpretation: A different perspective based on the self-organization theory of dreaming. Frontiers in Psychology, 9, 1553.
https://pubmed.ncbi.nlm.nih.gov/30190698/ -
Denis, D., French, C. C., & Gregory, A. M. (2018). A systematic review of variables associated with sleep paralysis. Sleep Medicine Reviews, 38, 141–157.
https://pubmed.ncbi.nlm.nih.gov/28735779/ -
Scammell, T. E. (2022, July 12). Clinical features and diagnosis of narcolepsy in adults. In A. F. Eichler (Ed.). UpToDate.
https://www.uptodate.com/contents/clinical-features-and-diagnosis-of-narcolepsy-in-adults# -
Sharpless, B. A. (2016). A clinician’s guide to recurrent isolated sleep paralysis. Neuropsychiatric Disease and Treatment, 12, 1761–1767.
https://pubmed.ncbi.nlm.nih.gov/27486325/ -
Olunu, E., Kimo, R., Onigbinde, E.O., Akpanobong, M.A.U., Enang, I.E., Osanakpo, M., Monday, I.T., Otohinoyi, D.A., & Fakoya A.O. (2018). Sleep paralysis, a medical condition with a diverse cultural interpretation. International Journal of Applied & Basic Medical Research, 8(3), 137–142.
https://pubmed.ncbi.nlm.nih.gov/30123741/ -
Hsieh, S. W., Lai, C. L., Liu, C. K., Lan, S. H., & Hsu, C. Y. (2010). Isolated sleep paralysis linked to impaired nocturnal sleep quality and health-related quality of life in Chinese-Taiwanese patients with obstructive sleep apnea. Quality of Life Research, 19(9), 1265–1272.
https://pubmed.ncbi.nlm.nih.gov/20577906/ -
Singh, S., Kaur, H., Singh, S., & Khawaja, I. (2018). Parasomnias: A Comprehensive Review. Cureus, 10(12), e3807.
https://pubmed.ncbi.nlm.nih.gov/30868021/ -
Denis, D., & Poerio, G. L. (2017). Terror and bliss? Commonalities and distinctions between sleep paralysis, lucid dreaming, and their associations with waking life experiences. Journal of Sleep Research, 26(1), 38–47.
https://pubmed.ncbi.nlm.nih.gov/27460633/ -
Kaczkurkin, A. N., & Foa, E. B. (2015). Cognitive-behavioral therapy for anxiety disorders: an update on the empirical evidence. Dialogues in clinical neuroscience, 17(3), 337–346.
https://pubmed.ncbi.nlm.nih.gov/26487814/ -
Denis, D., French, C. C., Schneider, M. N., & Gregory, A. M. (2018). Subjective sleep-related variables in those who have and have not experienced sleep paralysis. Journal of Sleep Research, 27(5), e12650.
https://pubmed.ncbi.nlm.nih.gov/29280229/














